Infections caused by drug-resistant bacteria such as Methicillin-resistant Staphylococcus aureus (yellow) are responsible for hundreds of thousands of deaths worldwide.Credit: National Institute of Allergy and Infectious Diseases/National Institutes of Health/SPL
A lack of funding and incentives for research into antimicrobial resistance (AMR) is causing scientists to leave the field, finds a report published on 8 February by the AMR Industry Alliance, an industry body that brings together more than 100 pharmaceutical companies and associations.
This ‘brain drain’ is a result of both governments and pharmaceutical companies investing less in developing antimicrobial drugs, the report says. It adds that the trend is particularly concerning given that AMR is a rising health concern worldwide.

The fight against antimicrobial resistance
Antimicrobials is a broad term for treatments that target disease-causing microorganisms, including bacteria, viruses, fungi and parasites. Many of the treatments have become ineffective because the pathogens they target evolve resistance to the active ingredients.
“The most pressing are antibiotics,” says James Anderson, chair of the AMR Industry Alliance Board in Geneva, Switzerland. The problem is global and involves a large number of infectious diseases. In 2019, bacterial resistance was responsible for 1.27 million deaths worldwide.
“When I first started, people knew resistance was a problem. And it was a growing problem, but it wasn’t recognized to the scale as we now know,” says Mark Webber, a bacterial geneticist at the Quadram Institute in Norwich, UK, who began studying the mechanisms of resistance in 1998.
Difficult economics
Table of Contents
Over the past decade, several major pharmaceutical companies have cut right back on AMR research, the report says. This is mainly because the market for antimicrobials — which are usually administered on a short-term basis, and often only after other treatments have failed — is less lucrative compared with those for treatments in areas such as cancer or HIV/AIDS. With each new antimicrobial, the risk of the target pathogen developing resistance is always present. “It’s a very difficult economic model”, says Webber.
Governments and public funding bodies are also committing less money to AMR research than to other areas, the report says. For example, the United States is one of the world’s biggest investors in AMR research, but allocates only one-quarter of the funding it gives to HIV/AIDS research.
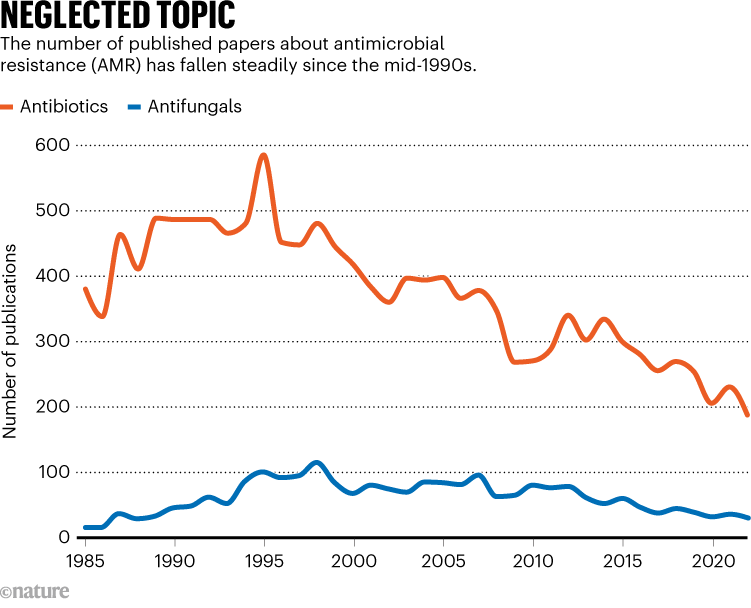
Source: Leaving the lab (AMR Industry Alliance, 2024)
The report also revealed a severe downward trend in the numbers of both researchers and published papers in the field over the past 30 years. Just 187 papers on antibiotics and 29 on antifungals were published in 2022, compared with 586 antimicrobial-related papers in 1995 (see ‘Neglected field’). And the alliance estimates that the workforce of AMR researchers shrank from around 3,600 researchers in 1995, to just 1,800 in 2020.
There has been strong trend for researchers to leave the field entirely after losing funding for their work, the report says. Of a sample of 150 researchers who worked at companies that stopped funding AMR research, around 60% went on to pursue research in other areas. By their second job change, only around 10% of these researchers remained in AMR.
Development void
The stagnating research in turn means that fewer antimicrobials are being developed. The US Food and Drug Administration approved almost half the number of new antibiotics each year throughout the 2010s as it did in the 1990s. This “development void”, says Webber, means that very few people in the field now have the experience of bringing a medicine to market from the early development stages. “There is that risk that a lot of that kind of knowledge is not at our fingertips,” he says.
Webber adds that more collaborative action and investment is needed between governments, pharmaceutical companies, health-care organizations and other stakeholders. “It’s not a lack of will. It’s a lack of ability due to the financial situation.”
The report suggests solutions, such as establishing incentives to motivate the development of antimicrobials, and training more early-career AMR researchers in an attempt to replenish the workforce. Some organizations are making progress in these areas, but more effort is needed on a wider scale, says Anderson. “What we’re doing is trying to make sure that the protective measures are put in place ahead of time.”
