
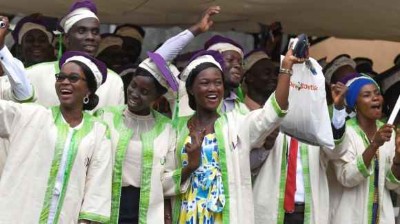
One in four Black men will be diagnosed with prostate cancer.Credit: Getty
Olugbenga Samuel Oyeniyi’s research at the University of Sunderland, UK, explores why many Black men do not seek help for symptoms of prostate cancer and uses Black peer educators to change mindsets in the community. March is Prostate Cancer Awareness Month in the United Kingdom.
What drew you to research?
Table of Contents
I worked in a hospital laboratory in Enugu in southeastern Nigeria after completing a bachelor’s degree in microbiology at Obafemi Awolowo University in Ile-Ife in 2006. Then I did a one-year master’s programme in biomedicine at the University of Portsmouth, UK, researching glioblastoma. My heart was set on academia, so in 2014, after working as a pre-clinical-trials research scientist based in industry, I started a PhD in applied microbiology at the University of Sunderland, looking at the Acanthamoeba parasite, which can cause blindness, among other things.
How did you get into prostate-cancer research?
In December 2020, I got a job as a senior scientist overseeing COVID-19 samples in a lab in Gateshead, UK, eventually becoming operations manager, which involved working with the University of Sunderland’s vice-chancellor, the local mayor and a member of Parliament. After the lab closed in May 2022, I saw an advert for a postdoctoral research associate in public health with a focus on prostate cancer. I automatically thought it was not for me — I was a clinical scientist dreaming of finding a cure for malaria. But then I read that one in four Black men will be diagnosed with prostate cancer, compared with one in eight white men, according to UK figures. That got my attention. I had a further look and it said one in 12 of those will die of it, compared with one in 24 white men. I thought, “Woah, this is affecting me” — I’m the eldest of four brothers. And not just me, but my community.
Nature Outlook: Prostate cancer
I started in September 2022, coordinating the research for Early Diagnosis of Prostate cancer for Black Men (PROCAN-B) project. It’s funded by Prostate Cancer Research, a London-based charity that supports research in this field in the United Kingdom and the United States.
Our aim is to reduce the obstacles to early diagnoses and save lives. What makes this work special is that it is research for Black men in the community, facilitated by Black men in the community, coordinated by a Black researcher.
How does the project work?
Our team includes public-health researchers, behavioural scientists, a psychologist, myself as project manager and two research assistants from the Black community who recruit the focus-group participants.
In October 2022, we created a community-led advisory and engagement group (also known as public involvement and community engagement, or PICE) made up of 13 Black men aged 47–63 from two parts of the United Kingdom: the northeast of England and Scotland. None of them had experienced prostate cancer personally, but one had a brother who was being treated for the disease.
We met three times to discuss the barriers to diagnosis and had a further three meetings to co-design interventions, such as community workshops to tackle some of these barriers to diagnosis. Then we had a further three meetings to train the group as peer facilitators to deliver the workshops. The first workshops took place in Sunderland and Glasgow in November 2023, with ten participants in each. We had feedback sessions a month later and used this information to refine the community workshops. We found that the men were interested and engaged in the pilot sessions — there were questions about every presentation slide.

Olugbenga Samuel Oyeniyi’s interests now lie in public health and epidemiology.Credit: University of Sunderland
So, we gave the men a piece of paper to write down their questions and we moved the Q&A part of the session with a general medical practitioner (GP), who was from the Black community, from the middle of the session to the end.
We held further workshops with 20 men each in Middlesborough and Glasgow in February. In Middlesborough, the men were so engaged. We were supposed to finish at 8 p.m., but there were still so many questions for the GP that we went on for another hour.
Why do Black men with symptoms sometimes avoid getting help?
Trust is a big issue: lack of trust in the statistics; in the health-care system; and in GPs. Men might have had negative experiences with gatekeepers such as the GP surgery receptionist, for example. There are also religious and cultural factors, such as social stigma.
The PICE group noted that talking about intimate and sensitive health issues such as prostate cancer is difficult for Black men because it can be embarrassing. Discussing intimate issues was a challenge related to sexuality and manhood. Group members also believed that Black men are raised to feel ‘super’, or stronger than women, which makes it difficult to show weakness and vulnerability.
You also identified structural racism as a barrier. Can you tell us about that?
Some of the participants described experiencing discrimination and racism in the health-care system. They feel they are treated differently and the same standards of care aren’t applied or don’t apply to Black people. One participant commented that health-care providers’ questions regarding medical conditions visible through changes to skin colour are written for white people and might not be applicable to a Black man. In another example, most of the statistics posted in bus-stop and train-station campaign ads say prostate cancer affects one in eight men. This is also part of structural racism — those are the figures for white men.
Your campaign involved video footage of British actor Idris Elba and US actor Morgan Freeman. Tell us how that helped.
These men are incredibly influential and in 2021 filmed Embarrassed, a powerful video from Black UK film director Steve McQueen, which was part of a separate campaign. We use it to inform the focus groups.
We also use videos of UK religious leaders — a pastor and an imam — and Black male survivors of prostate cancer. Other videos involve women, some of whom appeal to the men’s emotional side, saying “Your health is important to us and your families — look after your prostate health.”
How does PROCAN-B fit alongside other Prostate Cancer Research funding?
Our research is one of several projects the charity has funded as part of its racial-disparity funding call, particularly focused on Black men and prostate cancer. For example, one study from the University of Essex in Colchester, UK, has found that genetic mutations could help to explain why Black men are at higher risk of developing prostate cancer than are men of other ethnicities.
What is the future for the research — and for you?
If the workshops continue to be successful and our research shows they are making an impact, they could be rolled out across the country with a much larger group of people in a randomized controlled trial, depending on funding.
Career resources for African scientists
My current contract is due to end in August 2024. I want to continue with research, become a senior lecturer and do a master’s in public health, ideally at one of the top UK universities, potentially the University of Edinburgh or the London School of Hygiene & Tropical Medicine.
I believe the combination of laboratory studies and public-health research is key and crucial to comprehensive and extensive understanding of human health.
Eventually, my goal is to become a professor of public health and epidemiology, and to collaborate with researchers back home to address some of the health challenges facing Nigeria.
