Vaccines offer a potent armour against infectious diseases that once carried a heavy toll of mortality and morbidity, particularly among children. Gaps were already forming in that armour in the years before the COVID-19 pandemic. But amid stagnating vaccination rates, the pandemic acted like a shotgun, punching many more holes in humanity’s defences against preventable diseases such as measles.

Part of Nature Outlook: Children‘s health
The risks of allowing these infections to flourish are clear. Zimbabwe is currently working to contain a huge measles outbreak that claimed the lives of more than 750 children between April and October. And poliovirus has recently re-emerged in the United States after decades of successful elimination, prompting a state of emergency in New York.
The drop in vaccination rates is partly a direct consequence of the pandemic itself, which caused severe interruptions in public-health services and diverted resources. But it isn’t simply a crisis of access to vaccines. The failures and inequities in the global public-health response, coupled with politicization of the pandemic, have also undermined confidence in the institutions and people that coordinate and conduct immunization efforts.
As a result, global vaccination rates have hit their lowest point since 2008 — and getting back on track could be difficult. “We’re talking about tens of millions of lives that are at stake,” says Kate O’Brien, who heads the immunization programme at the World Health Organization (WHO) in Geneva, Switzerland. Rebuilding the trust lost during the pandemic will be a crucial step in pushing back against the global spread of otherwise preventable diseases.
Momentum derailed
Table of Contents
For much of the twenty-first century, vaccination efforts were moving in the right direction, continuing a trend that began in the 1970s. In 1974, the WHO initiated its Expanded Programme on Immunization, with the mission of ensuring worldwide access to vaccines against six deadly infectious diseases, including measles. By 2014, global vaccine coverage overall had reached 85% for many vaccine-preventable diseases, and some regions of the world had achieved remarkable successes. The Americas, says O’Brien, had eliminated polio, measles and rubella by 2015, even though those diseases continued to circulate elsewhere.
But vaccination is a continuous process, not a one-time victory, and further progress proved a challenge (see ‘Lost progress’). Jonathan Mosser, an epidemiologist at the Institute for Health Metrics and Evaluation at the University of Washington in Seattle, says that in the years leading up to the pandemic, “we really saw a stagnation of coverage for many of these long-established vaccines”. Furthermore, regional- or national-level statistics can mask considerable inequality at the local level. Duduzile Ndwandwe, a vaccinologist at the South African Medical Research Council in Cape Town points out that although the pre-pandemic coverage for routine childhood vaccines in South Africa was on the order of 85%, there were wide disparities within the country. “The poorest provinces like Eastern Cape, Limpopo and Mpumalanga were not doing that well,” Ndwandwe says. “They would be bordering on 60–70%.” This is well short of the 90% or more that is generally considered necessary for robust control of vaccine-preventable diseases.
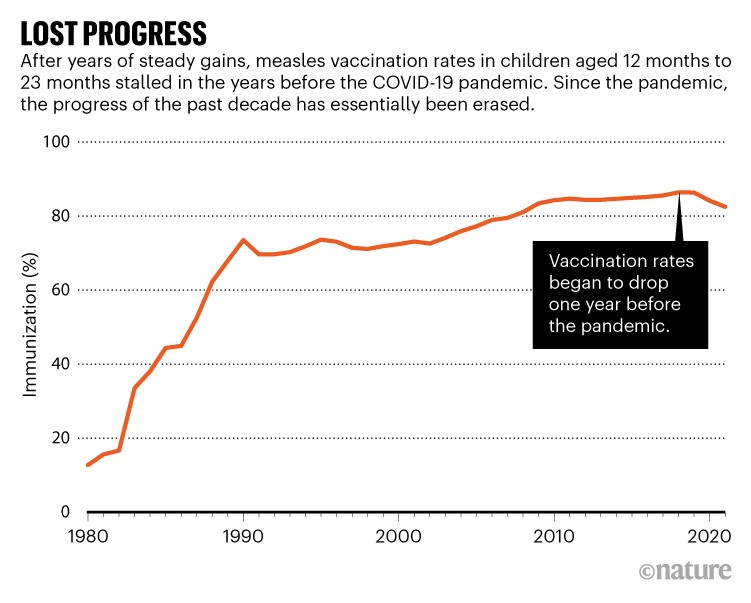
Source: The World Bank
By 2019, measles outbreaks were popping up with alarming frequency and posing a real global threat. “The scale of those outbreaks in 2019 was colossal, and we saw large increases in the number of deaths,” says David Durrheim, who studies public health at the University of Newcastle in Australia. “We saw countries being overwhelmed.” That year saw more than 200,000 measles deaths worldwide, a 50% increase over the 2016 total. There were a number of reasons for this backslide, including inadequate resources for vaccination programmes and the low priority given to immunization efforts in some countries. But rising vaccine hesitancy throughout the world was also an important factor, and the WHO named this trend one of the ten greatest threats to global health in 2019.
This perilous situation motivated the WHO to develop its Immunization Agenda 2030, which was announced in April 2020 with the goal of achieving 90% global coverage for the standard battery of childhood vaccines while also accelerating the introduction of new immunizations to low-income countries.
Delayed doses
But this announcement came mere weeks after the organization formally declared COVID-19 to be a pandemic. “It shut things down,” says O’Brien. “Compared with how many doses were given in the same month of the previous year, you just see this absolute plummeting in April, May and June of 2020.”
Routine paediatric vaccinations took a serious hit throughout the first year of the pandemic. Mosser and his colleagues combed through data from sources such as the WHO, and estimated that in 2020, COVID-19 led to 8 million to 9 million missed doses of routine childhood vaccines for diseases such as measles, rubella and diphtheria1. Some parts of Africa and Asia saw by far the sharpest drop in rates, but high-income countries in other regions also experienced dips at the start of the pandemic.
Much of this early impact was directly attributable to the strong measures taken to contain the spread of the SARS-CoV-2 virus, with many jurisdictions limiting travel, closing schools and restricting access to non-urgent medical care. But health-care providers were also struggling with limited capacity. “Resources and expertise were diverted from many sectors of health care, including immunization systems, to COVID response,” says Mosser. Even when there were no formal impediments to scheduling a visit to a health-care provider, social and psychological factors came into play that further undermined timely vaccination. “COVID kind of created the fear of even being in contact with the health-care services,” says Ndwandwe.
The pandemic also brought many targeted vaccination campaigns for children in resource-limited settings to a grinding halt. An analysis by the WHO found that by May 2020, nearly 60% of the 183 vaccination campaigns scheduled were either cancelled or delayed2.
As the immediate shock of COVID-19 passed, routine childhood vaccination efforts began to pick up steam again — particularly in higher-income countries. But even in wealthy regions, the pandemic amplified structural inequalities in the health-care system, and has left many underserved communities less protected against vaccine-preventable diseases. For example, Durrheim says that “in New Zealand, the second-dose coverage for measles has dropped to just above 80%, and that has fallen disproportionately in Māori, First Nations people and Pacific Islanders”.
In lower-income countries, the rebound has been more uneven. By the end of 2021, 16% of the vaccination campaigns scheduled by the WHO pre-pandemic had been cancelled or were still suspended, resulting in 382 million missed doses worldwide. O’Brien also notes that — somewhat paradoxically — the intense focus of the health-care community on delivering immunizations against COVID-19 sometimes meant the standard array of childhood vaccines were put on the back burner in favour of achieving pandemic control. “That’s why in 2021, we didn’t see the recovery that we thought was going to happen,” she says. Nevertheless, several countries, including Nepal, Bangladesh, Thailand and Pakistan, have been able to hold steady and maintain high coverage over the past three years by continuing to prioritize routine childhood immunization despite limited resources.
Confidence lost
But efforts to regain lost ground in vaccine coverage are also being jeopardized by other legacies of the pandemic, including the erosion of trust in governments and public-health institutions — a trend that the advent of COVID-19 vaccines has exacerbated rather than dampened.
Long before COVID-19 vaccines were even available for children, they had become a flash point for controversy — most notably, but not exclusively, in the United States. Daniel Salmon, a vaccinologist at Johns Hopkins University in Baltimore, Maryland, thinks some of the problems people have with the vaccine go back to its origins in Operation Warp Speed. This multi-billion-dollar US public–private partnership aimed to develop pandemic vaccines within an unprecedented, time frame. In particular, he is critical of the programme’s emphasis on speed without parallel planning around building public acceptance. “You’ve got to get people to want the vaccine,” says Salmon. “That wasn’t their goal.”

A worker with the Expanded Programme on Immunization prepares a measles vaccine at a health clinic in Nowshera, Pakistan.Credit: WHO/Asad Zaidi
Against the already politicized backdrop of the US COVID-19 response, the failure to generate public trust and enthusiasm around COVID-19 vaccines — particularly those developed with the relatively new messenger-RNA-based technologies — has created problems that will be difficult to solve. “Many people initially thought that by going on CNN and furrowing our brows, we would convince people to get vaccinated,” says Saad Omer, director of the Yale Institute for Global Health in New Haven, Connecticut, referring to the US news channel. “That’s not how vaccine persuasion works.” And when adults lack confidence in the vaccine, the likelihood of them immunizing their children plummets. As of October 2022, only 37% of eligible children in the United States had received even a single dose.
Although before the pandemic most US parents took their children to be vaccinated against multiple diseases to comply with school mandates, Salmon estimates that between one-third and one-quarter had serious concerns about the safety and necessity of these routine childhood vaccinations. “It’s the fence-sitters, the people who could be pushed over the edge, that worry me,” he says. This issue has become more salient in the context of COVID-19. For example, several reports have described cases of inflammation of the heart tissue — a condition called myocarditis — among adolescent boys receiving multiple shots of the mRNA vaccines3.
Although these cases are rare, mild and tend to resolve on their own, such safety concerns might shift the likelihood of vaccinating among parents who were already wavering. Framing these side effects relative to the much greater threat posed by COVID-19 itself is a challenge for governments and public-health organizations. “Public-health people need to be transparent,” says Katie Attwell, who studies vaccination policy at the University of Western Australia in Perth. “They do need to talk about the risks, and they need to contextualize the risks.”
The extent to which concerns about COVID-19 shots are fuelling hesitancy around other vaccines remains unclear. But some who study vaccine uptake are already concerned. “It’s going to take time to get data, but I would not be surprised if we see substantial drops in routine vaccines — especially in populations that have really been refusing COVID vaccines,” says Salmon. Omer’s research is already picking up some early indications of reduced uptake for the tetanus, diphtheria and pertussis vaccine among people in the United States who are pregnant. And even though these are still preliminary findings, he says “my concern is that this is sort of an iceberg where we’re just beginning to see the tip”.
There is also a clear political component to vaccine perception in the Western world. A 2021 survey4 of 1,745 US parents found that those who vote Republican are more than twice as likely to forego vaccinating their children against COVID-19 than parents affiliated with the Democratic party. For some people, at least, vaccine acceptance is deeply intertwined with political identity. An analysis5 of vaccine confidence in Europe found that vaccine hesitancy and refusal are closely tied with right-wing, populist politics.
And the possibility remains that this mistrust will spread globally. Heidi Larson, an anthropologist at the London School of Hygiene and Tropical Medicine, says “there is clearly a globally coordinated, very deep, negative network out there” exploiting pandemic-era mistrust to propagate and promote a broader anti-vaccine agenda through social networks such as Twitter and Facebook. In South Africa, Ndwandwe sees such vaccine hesitancy propagating mainly in more affluent communities that have the time and resources to find information — and misinformation — on the Internet. “TikTok is one of the more dangerous platforms that I have seen,” she says. “That’s where a lot of these things are happening.” In poorer communities without easy Internet access, the conversation is just as readily driven by radio broadcasts, religious leaders or poster campaigns, Omer says.
Overcoming hesitation
It would be a mistake, however, to simply attribute vaccine hesitancy to fear or misunderstanding of the science. As director of the Vaccine Confidence Project, a non-profit initiative based at the London School of Hygiene and Tropical Medicine focused on tracking global public sentiment around immunizations, Larson has been able to tease out some of the motives underlying the decision to vaccinate or not. According to her preliminary assessment of recent unpublished data from Africa and the European Union, many people are hesitant simply because they don’t see the importance of being vaccinated for diseases that they do not see as a real concern.
This is in keeping with Ndwandwe’s experience in South Africa. She says that mothers who already routinely engage with medical systems often trust their physician’s or nurse’s guidance that an immunization is important, even at the height of a pandemic. But the story is different in poorer communities, where people often need to make considerable trade-offs when seeking even routine care. “You’re talking about competing priorities here,” she says. “Do I want to travel 10 kilometres to go and sit in a clinic for the whole day, instead of going to a job that will pay me money and actually feed my kids?”
More from Nature Outlooks
The erosion of confidence in once-trusted authorities also plays an important part. But this can arise for a range of reasons — from bad-faith political arguments in Western nations to the long delay in providing COVID-19 vaccines to the world’s poorest countries. “If there’s one region that global health has really lost a lot of trust from, it’s Africa,” says Larson. “We’ve failed them big time, and that’s not going to be forgotten.”
Vaccine hesitancy or refusal is often the result of a complex mix of political, religious, social and cultural factors, as well as personal considerations that are highly specific to the individual. This calls for personalized solutions. “It’s mind-boggling that policymakers have such limited vocabulary to even have intelligent conversations about this,” says Omer. O’Brien emphasizes the importance of being “in constant listening mode” to understand the factors that are undermining coverage in a particular country, city or district. In many cases, this means targeted collaborations with local leaders who can effectively address their communities’ concerns.
This hyper-local process can also be scaled up, and a number of researchers are working on evidence-based tools that can guide families to informed vaccination decisions. Salmon and his colleagues have developed an online tool called Let’s Talk COVID Vaccines, which delivers tailored information based on each user’s concerns. A platform for encouraging immunization more generally, called Let’s Talk Shots, is expected to launch within weeks. Omer’s team has also devised a training strategy to help health-care workers to bolster COVID-19 vaccine uptake based on similar principles of targeted messaging, and he says that the United Nations children’s charity UNICEF is now adapting the team’s approach for international use. “It’s not just intuition — these are specific techniques derived from motivational interviews, and derived from experiments on how to correct misinformation,” he says.
Better data will also be crucial to helping the health-care community to quickly identify places where intervention is needed to prevent immunization levels from dipping too low. O’Brien says that the WHO has been working with member nations to adopt the agency’s district health information system, called DHIS2, which makes it easier to share granular within-country information about vaccine administration and coverage. But she also notes that the real challenge will be catching the ‘zero-dose’ children, most of whom live below the poverty line in settlements with inadequate housing and basic services, rural villages and conflict zones. “They’re born outside of a facility, they’ve never gotten a single vaccination, they’re sort of uncounted and unseen,” she says. “It’s really hard to plan to go out and vaccinate children who you don’t even know exist.” One of the goals of the Immunization Agenda 2030 is to reduce the number of zero-dose children by half, which the WHO estimates could save as many as 50 million lives over the next 10 years.
Now could be a unique opportunity to act. The public-health community’s response to COVID-19, including restrictions on travel and public gatherings, greatly limited the spread of many infectious diseases that would otherwise have run rampant. And despite crises such as the Zimbabwe measles outbreak, Durrheim says “we’ve reached in many countries the lowest measles case numbers that we’ve ever seen”. But as more and more countries are deciding — wisely or not — to put the pandemic behind them, the urgency of this mission only intensifies. “We either have to really invest now and close those immunity gaps,” says Durrheim, “or what will come will be devastating.”
