A wearable ultrasound device that attaches to the skin using a bioadhesive.Credit: Chonghe Wang
On a sunny day in April, one of us (C.W.) jogged along the Charles River in Cambridge, Massachusetts, with a series of small patches adhered to the skin. Each patch was an ultrasound sticker. On a smartphone, a live feed cycled through views of heart valves fluttering, muscles flexing, the diaphragm’s rise and fall and the flow of blood through arteries. Seamlessly connected to these hidden layers of physiology, the runner was able to watch the workings of their body in real time.
Wearable ultrasound devices such as these stickers still face many challenges. But they represent our vision for the future of ultrasound imaging and wearable devices1,2. Here we outline the promise of such technologies, and highlight remaining hurdles towards rolling out the devices in the next 5–10 years.
Imaging the body in real time
Table of Contents
In the field of personal health-care technology, wearables such as Fitbit and Apple Watch have become household names. These devices — small powerhouses of sensors and smart technology — can track steps, monitor heart rates and even perform electrocardiograms that once required a visit to the doctor’s office. They present biometrics in neat, digestible metrics, nudging people towards healthier lifestyles3. Wearable glucose monitors are also freeing people with diabetes from the frequent pricks of a needle, providing continuous readings of blood sugar.

An AI revolution is brewing in medicine. What will it look like?
Yet existing wearables generally collect data from only within millimetres below the skin’s surface. Other technologies can see far beyond this superficial layer — magnetic resonance imaging (MRI), X-rays and ultrasound, for example, can image internal organs. Of these, ultrasound is emerging as the front-runner in the race towards wearable adaptation.
Ultrasound operates on the principle of sonar, sending high-frequency sound waves into the body, which bounce back from internal structures to produce real-time images of dynamic processes such as a heart beating or blood flowing. Conventional point-of-care ultrasound imaging devices require a trained sonographer to press a handheld ultrasound probe against a patient who is static, meaning these devices are usually confined to hospitals and clinics. However, unlike X-rays, which require complex and potentially harmful ionizing radiation, ultrasound waves are relatively easy to produce, non-invasive and safe. These characteristics make ultrasound uniquely suited to a wearable form that is capable of continuous monitoring.
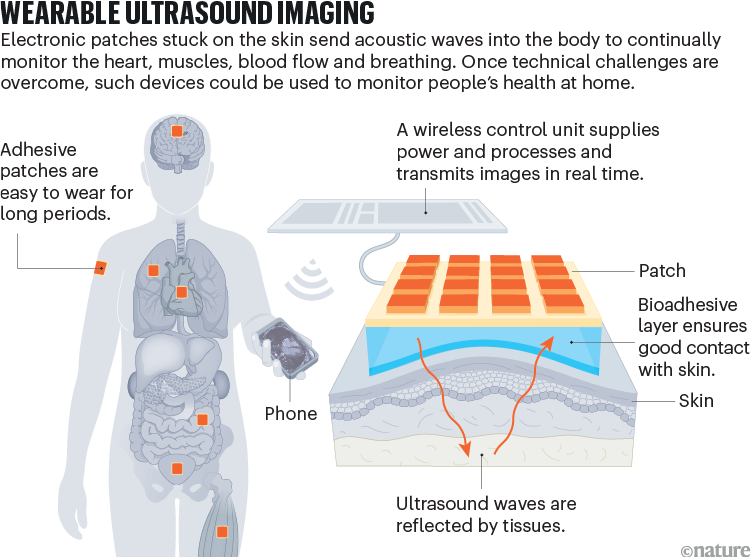
Our team has been exploring wearable ultrasound technology for the past few years1,2, alongside other groups of researchers pursuing the same goal4–11. The device we have developed is just a few centimetres long, attached to the skin using a bioadhesive and connected by wires to a pocket-sized battery and data-transmission system. This system wirelessly transmits clinical-level data to a tablet or smartphone (see ‘Wearable ultrasound imaging’). Our prototype, although still in its infancy, can deliver continuous, high-quality images of deep tissues. The battery life currently allows for minute-long videos to be taken intermittently: multiple times per hour over several days. We have not yet conducted clinical trials, but we expect to reach that stage in the next few years.
Source: C. Wang & X. Zhao
Wearable ultrasound systems hold great promise for transforming health care, supporting a shift towards preventive care and proactive health management. In clinical settings, they offer the potential for constant monitoring of high-risk patients, tracking fetal health in high-risk pregnancies or overseeing recovery after surgery. Beyond hospitals, these devices could bring diagnostic and monitoring tools to remote areas, making medical imaging more accessible and affordable in low- and middle-income countries. As the technology is refined, we foresee its integration into the daily lives of individuals to manage chronic conditions such as hypertension, or to enable early detection of heart failure, abdominal aortic aneurysms and deep vein thrombosis3.
The ability to image multiple organ systems continuously and simultaneously for extended periods also opens up opportunities to enhance our understanding of complex physiological and pathological processes. The data and insights obtained could substantially broaden our understanding of human biology and physiology at a systemic level.
Seven steps to market
Wearable ultrasound technology has already overcome some key technical challenges, but there are more ahead. These include refining the durability, flexibility and accuracy of these devices, as well as making them more comfortable to wear and extending their battery life.
Miniaturization. The company Butterfly Network in Burlington, Massachusetts, has made important strides in miniaturizing ultrasound technology. The firm has created a compact, ultrasound-on-chip platform for its Butterfly iQ device12, a small handheld ultrasound unit for use in clinics that was approved by the US Food and Drug Administration (FDA) in 2017. Although Butterfly iQ is not wireless or fully wearable, it demonstrates that high-quality imaging can be achieved with a compact ultrasound device.

Quantum sensors will start a revolution — if we deploy them right
Furthermore, recent advancements in ultrasonic-system-on-patch (USoP) technology have led to the development of fully integrated systems that combine ultrasound probes with miniaturized wireless control electronics in a soft, wearable format13.
Although the USoP technology cannot provide high-quality imaging, it allows continuous tracking of physiological signals from deep tissues and can operate wirelessly. The next step for these technologies is to integrate the capability of clinical-quality ultrasound imaging with fully integrated, wireless and wearable ultrasound devices.
Skin connection. To transmit and receive sound waves efficiently, an ultrasound probe needs to have a good connection with the skin. In the clinic, sonographers typically use a liquid gel to fill the gap between the probe and the skin, but the gel flows away quickly in wearable applications.
A few research groups have made the ultrasound probes stretchable to conform to the skin’s curved surface without the need for liquid gel9,11,13. However, the stretchable probes face an intrinsic challenge: because high-quality imaging relies on precise knowledge of transducer positions in the ultrasound probe, stretching it could markedly impair its imaging performance.
Our team has developed a bioadhesive ultrasound, which uses a thin, rigid ultrasound probe adhered to the skin with a specialized ‘couplant’ layer made of a hydrogel–elastomer hybrid that is soft yet tough, anti-dehydrating and bioadhesive1. This provides a robust and flexible connection between the probe and the skin, maintaining a good acoustic interface for high-quality imaging.

A team of doctors carries ultrasound equipment to a remote village in China’s Yunnan province.Credit: Zhang Jiayang/Xinhua via Zuma
Directionality. Another important challenge is ensuring that the ultrasound probe continues to point into the body in exactly the right direction even as the wearer moves around. We have been working on making our bioadhesive couplant adjustable so that the direction of the sound waves can be fine-tuned2. Currently, this requires an initial manual adjustment by clinicians to ensure that the probe is correctly aligned.
In practice, the bioadhesive ultrasound patches generally maintain their orientations well during typical activities, such as jogging and walking. However, they can require readjustment when subjected to more extreme movements, such as rolling over during sleep or if they are bumped.
Data analysis. Artificial intelligence (AI) can help with data analysis by interpreting the images produced and then alerting a clinician — or even the user — to potential problems and health concerns. AI-assisted data analysis is already used in clinical settings to interpret diagnostic data, including ultrasound images and X-rays. However, these systems face fresh challenges in wearable ultrasound, because the user’s movements introduce extra noise and variability into the data.
We are working on neural networks and generative AI models that enhance image clarity and reduce false alarms. These advanced AI algorithms are being developed to filter out motion artefacts and to improve the accuracy of continuous monitoring, ensuring that only significant health concerns are flagged for further examination.
Data transmission. Ensuring data privacy and developing robust wireless communication protocols that can handle the vast data streams from continuous imaging will be pivotal. Although our current system can handle intermittent data sampling, continuous data transmission remains a hurdle.

Skin sensors are the future of health care
The main challenges include developing secure and efficient data-compression methods and ensuring real-time transmission without compromising patient privacy. We are making progress, but this requires further research and development to improve bandwidth efficiency and ensure robust encryption methods to protect patient data.
Translation. Collaboration between scientists, engineers, clinicians and regulatory bodies is already happening and is essential for achieving the full potential of wearable ultrasound technology. Partnerships with technology innovators are driving advancements in components such as batteries and sensors, and collaboration with data scientists is refining the algorithms needed for operation guidance and data analysis.
As we advance wearable ultrasound technology, ongoing rigorous research, clinical trials and patient feedback will be crucial. These collaborations are fostering an environment in which innovative solutions can be developed and implemented, moving us closer to fully realizing the potential of wearable ultrasound systems.
Regulation. Whereas there are clear regulatory pathways for conventional ultrasound devices, establishing similar pathways for wearable ultrasound devices will accelerate their safe and effective integration into clinical practice. Currently, the FDA and other regulatory bodies are working to adapt existing regulations to account for the unique aspects of wearable technology.
The main challenges include creating standards for continuous monitoring, ensuring data privacy and securing wireless transmission to prevent unauthorized access to sensitive information. Addressing these regulatory gaps will be crucial to ensuring the safety and efficacy of wearable ultrasound devices in clinical settings.
Achieving these objectives will be key to transitioning wearable ultrasound from a promising prototype to an indispensable tool in personalized medicine. Ultimately, the widespread adoption of wearable ultrasound devices will transform not only how we monitor chronic conditions, but also how we understand the human body14.
