Researchers have restored1 circulation and cellular activity in the vital organs of pigs, such as the heart and brain, one hour after the animals died. The research challenges the idea that cardiac death — which occurs when blood circulation and oxygenation stops — is irreversible, and raises ethical questions about the definition of death. The work follows 2019 experiments2 by the same scientists in which they revived the disembodied brains of pigs four hours after the animals died, calling into question the idea that brain death is final.
The latest experiments are “stunning”, says Nita Farahany, a neuroethicist at Duke University in Durham, North Carolina. Although this study is preliminary, she says it suggests that some perceived limitations of the human body might be overcome in time.
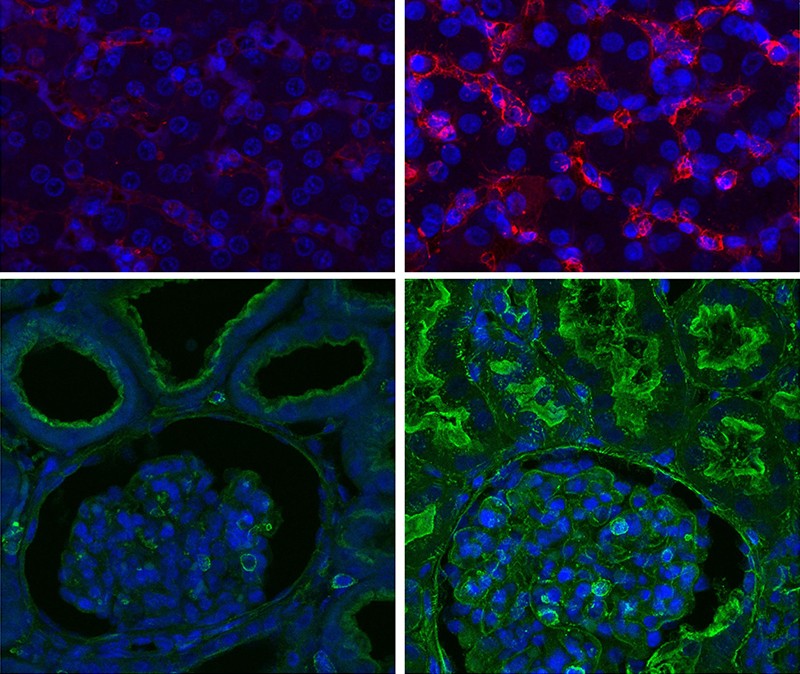
In the work, published on 3 August in Nature1, researchers connected pigs that had been dead for one hour to a system called OrganEx that pumped a blood substitute throughout the animals’ bodies. The solution — containing the animals’ blood and 13 compounds such as anticoagulants — slowed the decomposition of the bodies and quickly restored some organ function, such as heart contraction and activity in the liver and kidney. Although OrganEx helped to preserve the integrity of some brain tissue, researchers did not observe any coordinated brain activity that would indicate the animals had regained any consciousness or sentience.
As with the 2019 paper, the study is likely to reinvigorate a debate about the definition of death and the ethics of post-mortem organ donation. The authors warn that these results do not show that the pigs have somehow been reanimated after death, especially in the absence of electrical activity in the brain. “We made cells do something they weren’t able to do” when the animals were dead, says team member Zvonimir Vrselja, a neuroscientist at Yale University in New Haven, Connecticut. “We’re not saying it’s clinically relevant, but it’s moving in the right direction.”
Circulation restarts
Table of Contents
Nenad Sestan, a Yale neuroscientist and member of the team, predicted that these experiments might work in the light of the 2019 pig-brain study, because the brain is the organ most susceptible to oxygen deprivation. “If you can regain some function in a dead pig brain, you can do it in other organs, too,” he says.
To find out, he and his co-authors modified the BrainEx solution and the technique used for that study. “BrainEx was tailored for a specific organ, but we had to find a common denominator that works for all organs with OrganEx,” says Vrselja. In the OrganEx solution, the researchers included compounds that would suppress blood clotting and the immune system, which is more active elsewhere in the body than in the brain, he says.
Sestan’s team obtained pigs from a local farm breeder and monitored them for three days before sedating them, putting them on a ventilator and inducing cardiac arrest by delivering a shock to their hearts. After confirming a lack of pulse, they removed the animals from the ventilators. One hour after the pigs died, they restarted the ventilators and anaesthesia. Some of the pigs were then attached to the OrganEx system; others received no treatment or were hooked up to an extracorporeal membrane oxygenation (ECMO) machine, which some hospitals use in a last-ditch effort to supply oxygen to and remove carbon dioxide from the body.
After six hours, the researchers noticed that circulation had restarted much more effectively in pigs that received the OrganEx solution than in those that received ECMO or no treatment. Oxygen had begun flowing to tissues all over the bodies of the OrganEx animals, and a heart scan detected some electrical activity and contraction. But the heart had not fully restarted, and it’s unclear what exactly it was doing in those animals, says David Andrijevic, a neuroscientist at Yale University and team member.
The researchers also noticed that the livers of the OrganEx pigs produced much more of a protein called albumin than did the livers of pigs in the other groups. And cells in each of the vital organs of the OrganEx pigs responded to glucose much more than did the animals in the other groups, suggesting that the treatment had kick-started metabolism.
The findings are striking given how quickly after death decomposition begins, says Vrselja. Within minutes of the heart stopping, the body becomes deprived of oxygen and enzymes begin digesting cell membranes, leading to organs rapidly losing their structural integrity.
The researchers also found that more genes responsible for cellular function and repair were active across all major organs in the OrganEx group compared with the ECMO or no-treatment groups.
Involuntary movements
Curiously, only the OrganEx pigs started involuntarily jerking their head, neck and torso after receiving an injection of contrast dye that helped the scientists to visualize the animals’ brains following treatment. The researchers didn’t have a good explanation for the movements, noting that it’s unlikely that the impulses arose in the brain, given the lack of electrical activity. It’s possible that the movements arose in the spinal cord, which can control some motor functions independently of the brain, they say.
If the findings of cellular restoration can be replicated in animals and eventually in humans, their implications for human longevity could be as “profound” as the advent of CPR and ventilators, says Farahany. That’s because the technique could one day be used to preserve organs for transplantation — which are in short supply — or even resuscitation.
ECMO is currently used in an attempt to preserve the organs of some dead people for donation, or to try to resuscitate people following a heart attack. For these purposes, doctors typically need to start ECMO soon after the heart attack or death — and success rates can be low, depending on injury severity, says Sam Shemie, an critical-care physician at the McGill University Health Centre in Montreal, Canada.
Given the difference in how the pigs’ organs fared with OrganEx compared with ECMO, this is potentially a “landmark” study that could “significantly increase the number of organs that could be recovered for transplantation”, says Gabriel Oniscu, a transplant surgeon at the Royal Infirmary of Edinburgh, UK.
Before that can happen, further research to assess the viability of the recovered organs will be crucial, says Shemie.
Ethical challenges
With these potential implications come ethical challenges, says Farahany, especially if the technique could one day restore brain activity after death.
The researchers note that electrical activity in the pigs’ brains might have been absent because the solution they pumped through was colder (28 ºC) than normal body temperature, or because it included anaesthetic compounds and neuronal blockers that could have suppressed such signals. Farahany says it will be important for future researchers to test for any restoration of brain activity, particularly in light of the neck-jerking the researchers observed during the experiment.
The study also further emphasizes that death is not a moment but a process, making it challenging to come up with a uniform way to declare a person dead, says Arthur Caplan, a bioethicist at New York University. That means that the legal definition of death will continue to adapt as medicine continues to advance, he adds. “People tend to focus on brain death, but there’s not much consensus on when cardiac death occurs,” he says. “This paper brings that home in an important way.”